Precision Medicine

What is Genomics?
Your genome (also called your DNA) is the operating manual containing all the instructions that helped you develop from a single cell into the person you are today. Your genome guides your growth, helps your organs to do their jobs, and repairs itself when it becomes damaged. It's unique to you.
Advances in genome technology are leading to an understanding of cancer and new ways for diagnosing and treating many types of cancer.
Every pancreatic cancer patient is different. Patients who have received personalised treatment based on their biology have received benefits from targeted therapies.
Genomic Profiling
Genomic profiling of tumour tissue reveals your tumour’s biology, such as genes and proteins within the tumour. It is also sometimes called molecular profiling, tumour testing or biomarker testing.
Tissue sample is collected through a biopsy and analysed. Your oncologist may be able to use this information to make treatment decisions.
To sequence the DNA from cancer patients, DNA from both the tumour and healthy cells are compared. It allows us to detect two types of changes:
- Germline mutations - These are changes that are inherited from one's parents, or that occur spontaneously in very early development of the foetus
- Somatic mutations - These are changes that occur in the genome of cancer cells. Somatic mutations can be caused by environmental factors.
What does this mean for cancer patients?
Research tells us that each patient's cancer is different, yet we have treated them much the same. If we know more about the specific changes in the genome that led to someone's cancer, then we can look for more specific and effective treatments for their cancer.
We are moving toward treating cancers not by where they are found in the body, but by how their genomes have changed. The more we know about a patient's genome, the more we will understand their cancer and be able to offer them treatments that are more likely to work and improve their survival and quality of life.
Access to Cancer Profiling
One of the options we recommend is Omico.
They have received funding to provide free comprehensive genomic profiling (CGP) for 23,000 eligible Australians through its Cancer Screening Program called CaSP.
Everyone who has been diagnosed with pancreatic cancer regardless of cancer stage can access this program with a referral from their oncologist.
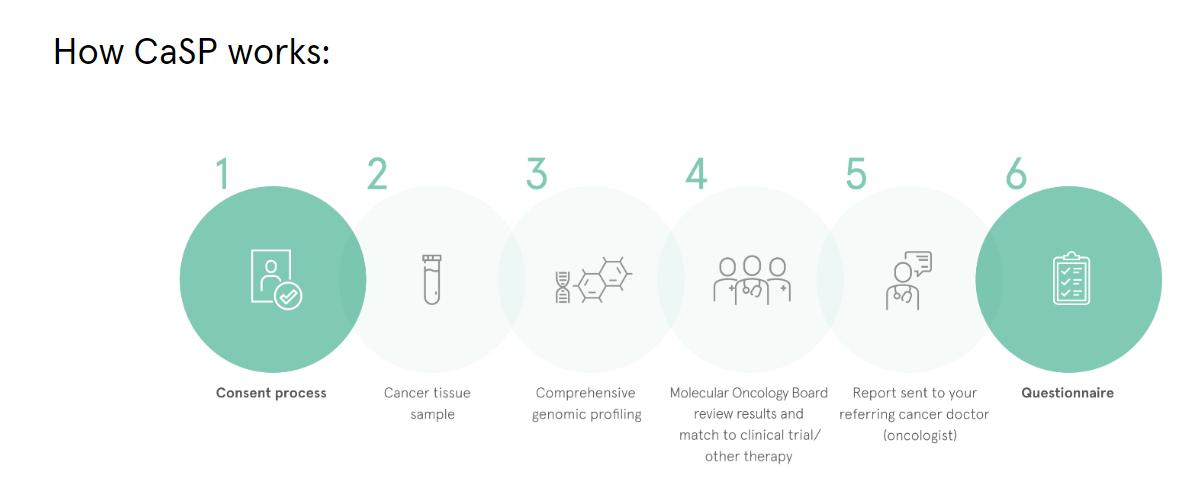
The process typically takes 8–10 weeks from when the patient has consented to participate for your referring doctor to receive the CGP and other reports. In urgent cases, as notified to the Omico CaSP team by your referring doctor, results will usually be provided in 5–6 weeks.
Centralising information about trial eligibility is key to attract more trials in Australia.
Genetic Testing for inherited mutations
It’s important to note that only about 10% of pancreatic cancers are considered hereditary. You may have been born with inherited mutations even if you don't have a family history of cancer.
The alterations to a person's DNA are the same throughout their whole body. So, this analysis is usually done on a blood or saliva sample.
FAQ
- I have been told my cancer is not curable, should I bother with CGP?
- What are the benefits of CGP?
- Do I need to do genomic profiling to access a clinical trial?
- Are there any alternatives to genomic profiling?
- Would a screening guarantee me to get a personalised treatment?
- Can insurers access my genetic results and use them against me?
I have been told my cancer is not curable, should I bother with CGP?
It’s never too late to do Genomic profiling. Even if a cure for your pancreatic cancer isn’t currently possible, CGP and treatment matching may offer valuable opportunities to optimise your treatment plan, reduce treatment side effects, manage symptoms, potentially extend your life, and maintain your quality of life. It’s about finding the best possible approach to support you through your treatment journey.
What are the benefits of CGP?
In the past medical treatments were designed for the average patient. Doctors would give cancer patients treatments, such as chemotherapy, not knowing if they would work for that person or not. We didn't know much about our genome then. As we have learnt more about the genome we have been able to start delivering medicine more precisely, to suit each individual.
Do I need to do genomic profiling to access a clinical trial?
No, there are trials that do not require people to have any particular molecular profile to enter. We suggest that you speak to your doctor and look at the Australian Clinical Trials Register.
Are there any alternatives to genomic profiling?
Your doctor will always provide you the best known treatment, called Standard Care. Genomic profiling is currently an addition to Standard Care, including the ability to access some clinical trials or other medications that may not be linked to where the cancer is in your body but may be linked to a known mutation in your tumour that may respond to a different type of treatment. You can find here more information about the Pancreatic Cancer Optimal Care Pathway.
Would a screening guarantee me to get a personalised treatment?
Not everyone referred to CaSP for genomic profiling will get a “fingerprint” result identifying a matching precision treatment. Sometimes, even if a precision treatment is identified there may be no clinical trial in Australia or the potential treatment may not be available. You and your doctor can discuss which treatment options might be best for you.
Can insurers access my genetic results and use them against me?
It was announced in September 2024 that life insurers will be banned from using genetic testing to refuse cover. Find out more here. This is a big step forward for people who would like to have genetic testing to manage their risk and treatment of disease.